- Details
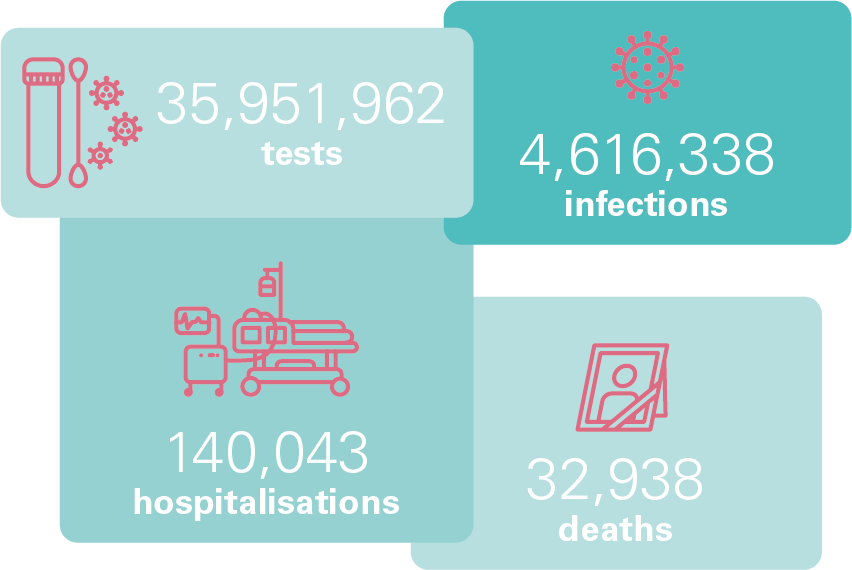
- Number of new infections and number of tests
- COVID-19 patients in general hospitals
- Total number of deaths due to COVID-19
- Vaccination
[1]Source: Sciensano. This covers dates from the beginning of the pandemic to 31/10/2022
- Details
The postponement of non-essential care and the treatment of COVID-19 patients had a considerable impact on hospital activity in 2020. We find that the number of stays decreased by 16% in general hospitals and by 7% in psychiatric hospitals[1]. The greatest decrease, by 23%, can be observed in the number of surgical day hospitalisations. The strong reduction in the number of outpatient contacts with the emergency department could be an indirect consequence of the measures taken in 2020. Indeed, especially during the first wave, social contacts were greatly limited, teleworking became the norm, and work in some sectors came to a complete halt. As a result, fewer accidents occurred, which led to a lower number of contacts with the emergency department.
EVOLUTION IN THE NUMBER OF STAYS PER TYPE OF STAY
Both in March and in November 2020, we see a clear effect of the measures taken regarding the postponement of non-essential care. There is a considerable drop in the number of stays for all types of hospitalisations. At the restart of day hospitalisation and classic hospitalisation in May 2020, we observe that the number of stays remains below the level of the number of stays in January and February 2020.
In November 2020 – when the second wave of COVID-19 hits – we once again observe a considerable reduction in activity as a result of the measures taken. Although at that time this was not part of the measures adopted, we also see a reduction in non-surgical day hospitalisations.
EVOLUTION IN THE WEEKLY NUMBER OF ADMISSIONS PER TYPE OF STAY
During the period from 14/3/2020 to 4/5/2020[2]we saw that the total number of hospital stays more or less halved in 2020 compared to the median of the number of stays in the years 2016 to 2019. The greatest reduction could be observed in surgical day hospitalisations, where only 11% of expected stays took place. Classic hospitalisations, non-surgical day hospitalisations and ambulatory contacts through the emergency department saw a drop to 55%, 50% and 61%, respectively, compared to the activity in the previous four years.
In the period from 26/10/2020 to 27/11/2020, 75% of expected stays took place, compared to the activity in the period from 2016 to 2019. Once again, we observe the greatest reduction in surgical day hospitalisations, where 46% of expected stays took place, followed by ambulatory contacts with the emergency department (64%), classic hospitalisation (71%), and non-surgical day hospitalisation (95%).
PERCENTAGE OF THE NUMBER OF STAYS IN THE REFERENCE PERIOD COMPARED WITH THE MEDIAN OF THE 4 PRECEDING YEARS BY HOSPITALISATION TYPE [3]
In the two periods where non-essential care was postponed, one third of hospitalisations of non-COVID-19-patients was a contact for chemo or immune therapy (28%), 11% a stay relating to a form of chronic pain, and 6% of stays were for giving birth.
Impact of the pandemic on the nursing workload
In the graph below, an overview is given of the general nursing workload for patients with and without a COVID-19 diagnosis. The general nursing workload gives an idea of the care needs of the patient. These are determined based on how many nursing care services were performed, how much time was necessary to provide the care services, or the degree of nursing competency required for the care services.
PERCENTAGE OF NURSING WORKLOAD
FOR PATIENTS WITH AND WITHOUT COVID-19 INFECTION
For 46% of COVID-19 patients, the nursing workload is high to very high, which means that the nursing workload amounts to more than 150% of the nursing workload for the average patient[4]. In addition, for 10% of patients, the nursing workload is even more than 3 times as high as for the average patient. By way of comparison, we find that only 25% of patients without COVID-19 infection are classified into the categories high to very high.
[1]Source: MHD and MPD, Data and Policy Information Service, FPS HSFCE. At the time of publication, our services only have data for 2020 for all stays (both COVID-19-related and non-COVID-19-related) in general and psychiatric hospitals.
[2]The reference periods chosen are the periods in which the HTSC Committee asked to postpone non-essential care. Hence, these periods do not comprise the entire COVID-19 wave. Due to the nature of the registration, these figures cannot be shown for the evolution of the number of stays in psychiatric hospitals.
[3]For stays in psychiatric hospitals, due to the manner of registration, no comparison can be made based on the number of stays in the chosen reference periods. For this reason, these stays are not included in this graph.
[4]Patients are classified into 5 categories: ‘Very low’: the care workload amounts to max. 25% of the care workload for the average patient; ‘Low’: the care workload amounts to 25 to 50% of the care workload for the average patient; ‘Medium’: the care workload amounts to 50 to 150% of the care workload for the average patient; ‘High’: the care workload amounts to 150 to 300% of the care workload for the average patient; ‘Very high’: the care workload amounts to more than 300% of the care workload for the average patient.
- Details
Impact of the COVID-19 pandemic on 1733 calls
Telephone calls in the context of non-plannable care in Belgium are organised via 2 central telephone numbers. Calls for urgent medical assistance via 112 are responded to by an operator in an emergency centre. Non-urgent medical calls to 1733 are responded to by an operator in an emergency centre or forwarded to an out-of-hours GP service.
CHANGE IN NUMBER OF DAILY CALLS TO 1733
The number of calls made to the number 1733 reached a record high over the weekend of 14 and 15 March 2020. This peak was due to the fact that many members of the public called this number for additional information on COVID-19 rather than because of a medical problem. The emergency centres experienced unprecedented levels of activity that weekend. Every effort was made to answer all calls. Additional staff were called in, support was provided by the medical directorates and helplines with GPs were set up.
Following the weekend of 14 March 2020, it was decided to set up call-forwarding to the 0800 coronavirus information line when calls were made to the emergency centres. This would filter out the calls to the emergency centres where people only wanted to receive information on COVID-19. We observed that people continued to use the emergency numbers for a long time to obtain information on COVID-19, with questions about vaccinations, test results, etc.
After the peak in March 2020 we have observed a few more increases in the number of calls to the number 1733. These increases often coincide with an increase in the number of infections and with the moments at which decisions were taken and communicated by the Consultative Committee.
Impact of the pandemic on the intervention time of ambulances

When a call for emergency assistance is received in a 112 centre, an ambulance service is alerted to pick up the patient in question at the intervention site and transport them to the hospital. It was found that – primarily during the first wave of COVID-19 – the median ambulance departure time (i.e. the time between the call made to the ambulance by the 112 centre and the departure of the ambulance to the intervention site) increased significantly for a brief period[1]. This could be due to the fact that the emergency service workers had to put on their protective clothing just before their departure, which took more time due to the COVID-19 measures. As they got more used to this and the number of COVID-19 infections fell, the departure time once again decreased. After a slight increase during the second wave of COVID-19, the departure time remained stable.
IMPACT OF COVID-19 ON AMBULANCE DEPARTURE TIMES
In addition, we can observe that the weekly median length of time that an ambulance crew is present at the intervention site shows a clear increase in the periods leading up to the various COVID-19 waves.[1][2].This in turn can be explained by the fact that due to the higher risk of infection and the COVID-19 measures in force, a more cautious approach was taken in taking care of patients. This has an impact on the duration of interventions at the intervention site. Another explanation could be that fewer non-essential interventions were carried out during the COVID-19 waves. Consequently, it could be assumed that there were more interventions for patients with more severe conditions, which could explain the rise in the weekly median.
IMPACT OF COVID-19 ON TIME SPENT BY AN AMBULANCE AT AN INTERVENTION SITE
[1]Source: AMBUREG, Data and Policy Information Service, FPS HSFCE (6.48% of primary interventions were not taken into account due to missing values).
It should be noted that the interventions were taken into account until 31/10/2022. As a result, only a few days (i.e. 29/10/2022– 31/10/2022) were included in the last bar in the graph instead of a full week. It should also be noted that there is a fall in the number of interventions in the 30/12/2020 and 31/12/2021 segments. This is because only one or two days were taken into account in these segments (30/12/2020 and 31/12/2020, on the one hand, and 31/12/2021, on the other hand).
[2]Source: AMBUREG, Data and Policy Information Service, FPS HSFCE (23.60% of primary interventions were not taken into account due to missing values).