- Details
What are locoregional networks?
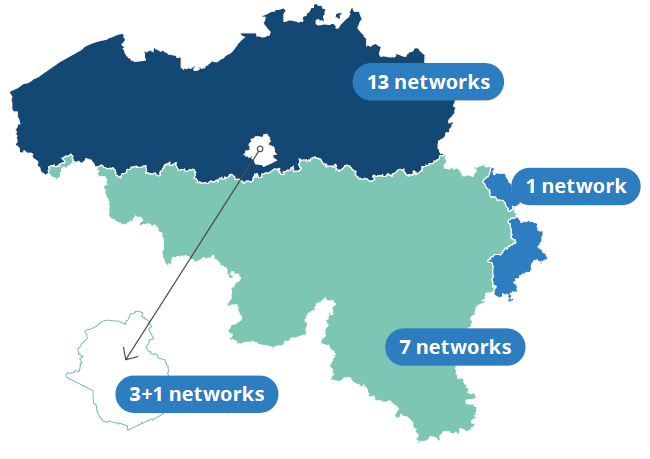
A locoregional hospital network is a cooperation between at least two hospitals, which are geographically contiguous, in the area of (basic) care. Since 1 January 2020, every hospital has been required to be part of one, and only one, locoregional hospital network. A maximum of 13 networks may be formed in Flanders, eight in Wallonia and four in Brussels. The way in which hospitals organise the management of the locoregional care provision within their network is determined by the hospital network itself.
Learn more? https://etaamb.openjustice.be/fr/loi-du-28-fevrier-2019_n2019040712
Working together on care assignments
The basis of the reform introducing locoregional hospital networks is twofold:
‘Care should be provided in the vicinity when possible, specialist care where needed.’
In other words and on the one hand, the government wants to ensure that care is provided as close to home as possible. On the other hand, from a quality perspective, the government wants to concentrate highly specialised care. This will also lead to a more efficient use of resources.
A subdivision of care has been established that divides healthcare into locoregional and supra-regional care assignments.
1. Locoregional care assignments
These are the care assignments that may be offered in any locoregional hospital such as an emergency department and a geriatric or paediatric department. These are services that are needed to guarantee basic care for conventional surgical procedures and medical conditions. Moreover, locoregional care includes services that require patients to come to the hospital regularly for a certain period of time, for example kidney dialysis, the oncology care programme and stroke care. These types of care should be offered in every hospital network, but not in every hospital.
2. Supra-regional care assignments
These are care assignments for a small group of patients, which require considerable expertise and/or investment. These types of care should not be offered in all networks but must be concentrated in supra-regional reference centres. These include specialist stroke care and burn centres.
The goal is to create an appropriate framework that encourages collaboration within the sector. In the next phase, hospitals within the network may choose to bring together different services or care packages in the form of shared services. In this way, resources can be used more efficiently, for example, by making group purchases or by operating heavy equipment together.
As a result of quality improvement and specialisation, locoregional hospital networks will become more attractive to healthcare providers and patients. Mutual cooperation between reference centres, which offer supra-regional care, will allow patients to receive further follow-up in a hospital near their place of residence after undergoing a treatment.
- Details

The general hospitals can be subdivided into three different types[1]:
As of 01.01.2023, 30% of the 103 hospitals in Belgium are public, i.e. managed by a public authority (a municipality or an inter-municipal, provincial, regional authority, etc.), and 70% are private and run as non-profit organisations. Historically, the latter owe their existence to religious orders, mutual societies, free universities or former company hospitals. However, given the large number of hospital fusions in recent decades, many current institutions are a legacy of both the public and private sectors. The Hospitals Act makes no distinction between the public and private sectors. Consequently, the provided government funding is identical.
[1] This report zooms in on general hospitals under federal jurisdiction. It leaves out psychiatric hospitals (which provide care exclusively to people with mental disorders).
- Details
The activities of hospitals are organised into services, functions and care programmes.
Services group together activities that are linked to a specific location within the hospital. A distinction is made between hospitalisation services, where patients reside during their stay in hospital, and medical or medico-technical services, where certain specific services requiring special expertise or equipment are provided. Medical services include transplant centres or centres for burn victims. Medical-technical services include medical imaging services (CT scanning, NMR, Pet-Scanner, etc.), human genetics centres, radiotherapy services and kidney dialysis centres.
Functions are hospital activities made available to all hospital departments. Several functions are subject to specific standards and controls by the competent community or region. Functions include hospital pharmacy, palliative care, intensive care and emergency department, hospital blood bank, mediation, pain management and the clinical biology lab, amongst others.
Care programmes can be defined as an organisational framework for implementing ‘care pathways’ for a specific target group. They are the result of an arrangement between the hospitalisation services, medical or medico-technical services and functions that are necessary in order to provide high-quality care.
There are currently various care programmes:
- The care programme for ‘cardiac pathology’
- The care programme for ‘reproductive medicine’
- The care programme for cancer patients
- The care programme for children
- The care programme for geriatric patients
- The care programme for ‘stroke care’.
Find out more about the location and services offered by the different hospitals: https://www.health.belgium.be/fr/sante/organisation-des-soins-de-sante/partage-de-donnees-de-sante/institutions-de-soins
Types of hospital services
Each service within the hospital must be accredited and meet specific standards, including minimum bed capacity, the required level of activity, technical equipment and the number of providers of medical, paramedical and care services.
Each service is allocated an index or identification letter referring to the subgroup of patients concerned. To be able to provide a better overview, we can group the different types of services according to the nature of the conditions generally treated there.
- Acute beds: for short stays, i.e. stays that do not require long-term treatment: e.g. surgery (index C), internal medicine (index D), paediatrics (index E), care of premature infants (index NIC), maternity (index M).
- Geriatric beds: for the care of geriatric patients (index G).
- Chronic beds: for longer-term hospitalisations or for patients requiring chronic treatment: rehabilitation (index S1 for cardiopulmonary pathologies, S2 for locomotor pathologies, S3 for neurological pathologies, S5 for chronic polypathologies and S6 for psychogeriatric pathologies) and beds for palliative care (index S4).
- Psychiatric beds and places: for the care of patients with mental disorders, possibly only during the day or at night: such as beds or places for the observation and neuropsychiatric treatment of adults (index A, A1, A2, T and T1) or of children (index k, k1 and k2).
Evolution in the number of accredited hospital beds
Population ageing and innovation in healthcare are reflected in the changes in the number of accredited hospital beds. Since 1995, we have seen a decrease in the number of accredited ‘acute’ hospital beds (-24%). The reason for this is that over the years, patients have to spend less time in the hospital for certain illnesses and procedures. The case of geriatric (+29%), specialist (+370%) and psychiatric beds (+67%)[1] shows a shift in the opposite direction. In these areas, an increase in the number of beds is observed since 1995. This can be explained in part by the ageing of the population. Overall, we have observed a decrease of 2,395 beds (-4%) in Belgian hospitals. Between 2010 and 2015, we have seen an increase in accredited beds as a result of mergers between general and specialist hospitals[2].
Evolution of the number of accredited
hospital beds
The geographical distribution of accredited hospital beds
per 100,000 inhabitants
The Brussels-Capital Region has the highest number of beds per 100,000 inhabitants. In second and third place we find West Flanders and Hainaut, respectively. Walloon Brabant and Flemish Brabant are the provinces with the lowest number of beds.
Number of accredited beds per
100,000 inhabitants by province and the Brussels-Capital Region
[1]Frozen beds will be counted given the accreditation for this is maintained.
[2]Source CIC: 01/01/2023
- Details
Number and percentage by category of professionals (in terms of FTEs) in 2020
The volume of FTEs (= Fulltime equivalents) increased by 4,198 FTEs (+3.22%) over the past 5 years. The largest increase is observed among medical salaried personnel (+26.62%). This increase is mainly due to the increase in the number of physician specialists in training.
Evolution of the volume of FTEs between 2016 and 2020
[1]Source: Finhosta