- Details
With the signing of the ‘Guide to Improved Mental Health Care through the Realisation of Care Circles and Care Networks’ by all competent Ministers, the Interministerial Conference (IMC) Public Health kicked off the reform of adult mental healthcare in 2010[1]. Various pilot projects were launched in which mental healthcare networks (MHC networks) were set up and systematically expanded. An evaluation was carried out in 2017 and a number of networks were redesigned, which left 20 MHC networks for adults. Currently, every Belgian municipality is part of one of the 20 MHC networks.
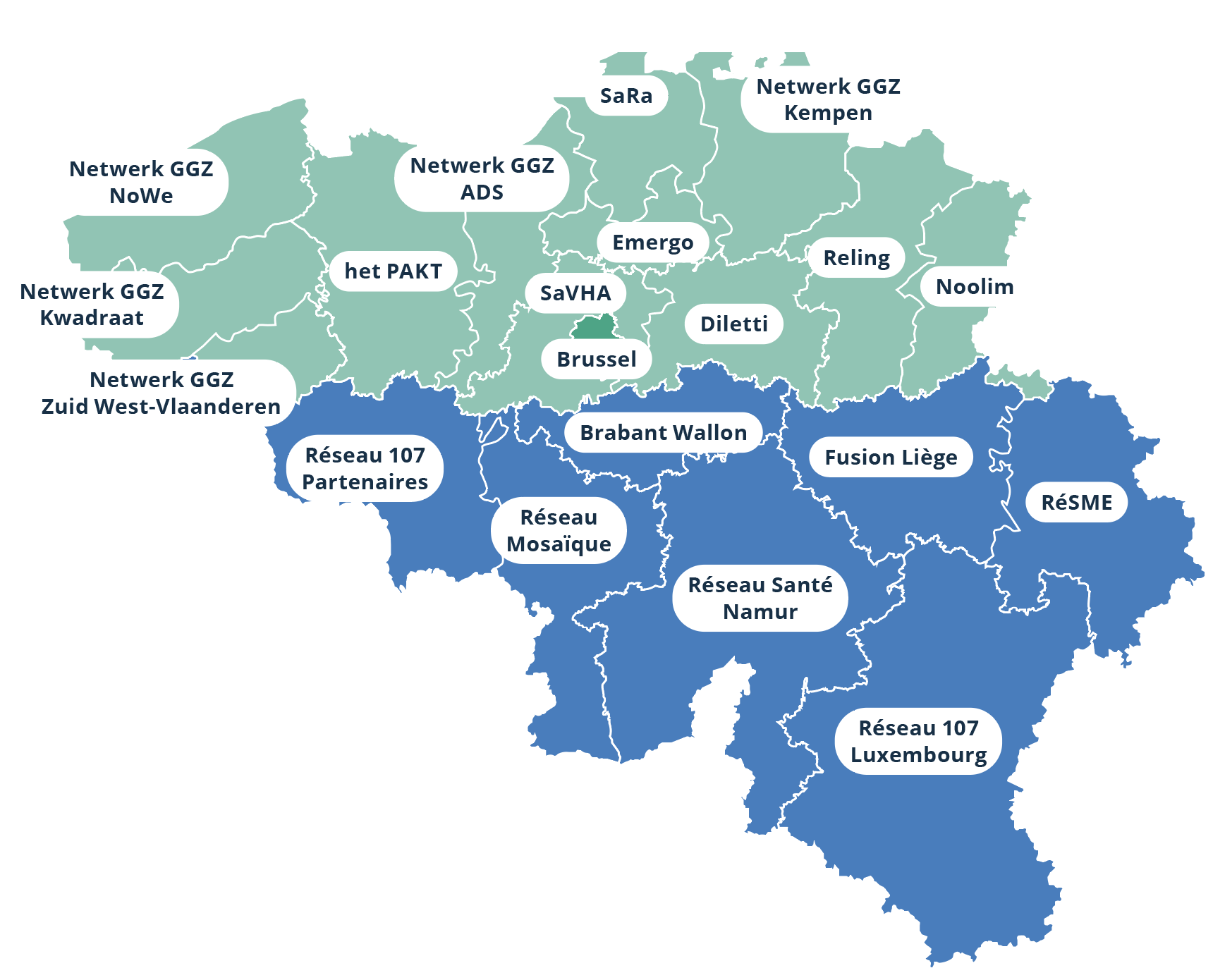
A policy for working towards a more community-based mental health care was deliberately chosen because it can be seen that home-based care, possibly combined with short intensive residential care, leads to better outcomes for patients and their families. What follows highlights some topics for which the federal government has jurisdiction, whereby we analyse the offer and activity in PH, PDGH, and in relation to internment. Finally, the nature of treatments in the context of substance abuse is discussed.
Learn more? www.psy107.be
[1] It has already been stated that the care offering for the elderly should be a continuation of the reform for adults and consequently be expressly chosen to be an addendum/an update guide 2.0 to the already existing guide for adults so that it is responsive for all adults.
- Details
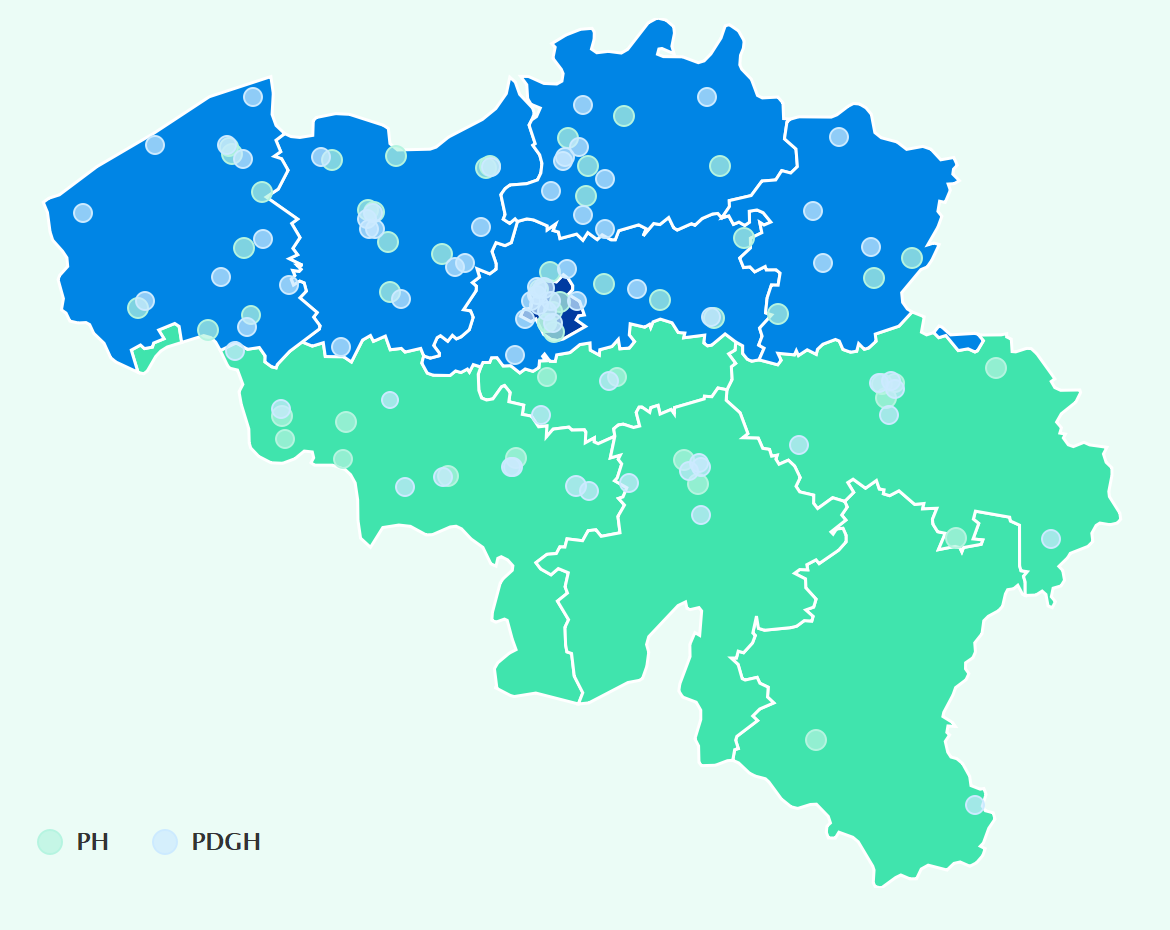
Psychiatric hospitals (PH) and psychiatric departments within general hospitals (PDGH) are part of the mental healthcare networks. The organisation and activity of these institutions is outlined below.
Number of hospitals according to number of accredited beds for adults with psychiatric problems (01/01/2023)
|
Distribution of hospitals In Belgium are 71 PDGH and 51 PH serving adults with psychiatric problems[1]. Almost 90% of the PDGH have less than 100 adult beds. In contrast, 80% of the PH have more than 100 beds.
|
Types of beds and places for residential and partial hospitalisation
Psychiatric institutions are often divided into different units according to the therapy or pathology provided. In each unit, a number of accredited beds are available with a specific index reflecting the type of care provided.
In psychiatric care, it is possible for a patient to be admitted to a psychiatric service where the patient stays in the institution day and night. This is referred to as residential hospitalisation. In addition, it is possible that a patient stays in the institution only during the day or only at night. This is referred to as partial hospitalisation.
Residential hospitalisation
- Beds for acute care (index A): The neuropsychiatry service for observation and treatment (day and night) of patients aged 15 and over in need of urgent care;
- Beds for chronic care (index T): The neuropsychiatry service for treatment (day and night) of long-term and chronic problems in adults, with a focus on social re-adjustment. In this document, beds for the neuropsychiatric treatment of geriatric patients (index Tg) are included in this category;
- Beds for specialised care (index Sp 6): Specialised service for treatment and rehabilitation for patients with psychogeriatric and chronic conditions;
- Beds for intensive care (index IBE): Intensive treatment unit for adult patients with severe behavioural disorders and/or aggressive adult patients.
Partially hospitalisation
- Places for acute care for day hospitalisation (index a1): the neuropsychiatry service for observation and treatment for day hospitalisation of adult patients in need of urgent care;
- Beds for acute care for night hospitalisation (index a2): the neuropsychiatry service for observation and treatment for night hospitalisation of adult patients in need of urgent care;
- Places for chronic care in day hospitalisation (index t1): the neuropsychiatry service for day hospitalisation for adults with long-term and chronic problems;
- Beds for chronic care in night hospitalisation (index t2): the neuropsychiatry service for night hospitalisation for adults with long-term and chronic problems.
Number of accredited adult beds (01/01/2023) and number of decommissioned beds
This is possible based on Article 107 of the Hospital Act which states that (translation) “The King may provide for specific funding methods to enable, on an experimental basis and limited in time, the prospective and programme-orientated funding of care circuits and networks”. Mental health reform is often referred to as ‘Project 107’ due to these regulations.
The staff freed up by the decommissioning of the beds can be deployed in alternative forms of care provision. In practice, these are mobile teams for specialised care in the home environment or more staff are deployed to residential care.
The highest proportion of beds were decommissioned from among chronic care beds (58.7% in t2, 30.1% in T and Tg).
Relative to population, the Flemish region has the largest supply of psychiatric care in PH and PDGH with 111 residential care beds, 26 day hospitalisation places and 2 night hospitalisation beds per 100,000 inhabitants, respectively. This equates to a total of 139 beds per 100,000 inhabitants in the Flemish Region[3]. In the Brussels Capital Region and the Walloon Region, the total supply is smaller, with 112 and 115 beds and places per 100,000 inhabitants, respectively.
Number of accredited beds and places minus number of decommissioned beds for adults per 100,000 inhabitants
If we look at the evolution of the number of beds by type of care, we see that there was a shift from beds for residential, chronic care to beds for acute care. This reflects the efforts made in the context of the reforms to mental healthcare, stipulating that no new beds could be created without phasing out other accredited beds.
We have noted a 6.4% decline in adult psychiatric beds over the past 20 years[4]. The foremost decrease of 39.5% can be seen in chronic care beds (T, Tg). The number of beds and places for chronic day and night hospitalisation also fell sharply (19%). Both decreases arose as a result of both the decommissioning of beds via Section 107 and the disappearance of registration.
In addition, we have seen an increase for both acute and specialised beds (A by 17.2% and S6 by 9.5%). The number of places for acute day and night hospitalisation (a1 and a2) is clearly increasing (+35.6%). In practice, this is reflected in the change in the offering from more chronic care to acute treatment and day therapy.
Evolution in the number of accredited beds and places for adults in PH and PDGH minus number of decommissioned beds
|
Characteristics of hospital stays In 2021, a total of 119,501 stays (residential and partial) were accredited in psychiatric services for adults in PH and PDGH[5]. Of these, 61,412 were stays in PH and 58,089 in PDGH. From 2007 to 2019, we observed an increasing trend that was interrupted as a result of the measures taken in the context of the COVID-19 pandemic. Nevertheless, there is a 4.5% increase in the number of stays in PH and 17.0% in PDGH over the period from 2007 to 2021.
|
Evolution in the number of hospital stays in psychiatric services for adults in PH and PDGH
|
Number of stays of men and women in PH and PDGH in 2021
|
|
In 2021, 58,470 men and 61,012 women stayed in PH and PDGH[6]. Therefore, both genders accounted for almost an equal number of stays. We can, however, observe a clear difference in the type of facility where a man or a woman is treated for his/her problems. Namely, we see that more women are admitted to a PDGH, whereas more men are admitted to a PH. |
Number of stays by age group in PH and PDGH in 2021
|
|
46.06% of stays in adult services in PH and PDGH concern patients between 41 and 64 years old[7]. 40.40% concern patients between 19 and 40 years old. The distribution in PH and PDGH is similar. |
Number of stays by type of hospitalisation in 2021
|
|
80.2% of stays take place in residential acute care services (A), while 14.2% take place in acute services for day hospitalisation (a1). This figure has doubled over the last 15 years. |
Duration of stay in psychiatric services for adults in PH and PDGH in 2021
|
|
A stay in an adult psychiatric service in a PH is generally longer than a stay in a PDGH[8]. Almost 80% of the stays in the latter last less than one month, while one third of the stays in PH last between one and three months. |
Evolution in the number days spent in PH and PDGH in adult psychiatric services
|
|
The number of days of hospitalization in PH and PDGH in adult psychiatric services decreased by 10.5% between 2007 and 2021 from 5,068,824 to 4,537,628 days. |
More information about the characteristics of hospital stays: https://www.health.belgium.be/fr/activite-de-soins-au-sein-des-etablissements-psychiatriques
Top 10 main diagnoses in 2021
|
A diagnosis in the event of psychiatric hospitalisation is rarely unequivocal; there is usually a combination of problems. If we take the main diagnoses of patients in PH and PDGH as the basis, we find that depressive disorders were the most common in 2021. Two-thirds of these stays took place in a PDGH. A main diagnosis of problems related to alcohol abuse follows in second place. |
|
More information about diagnoses made during admission to PH or PDGH: https://www.health.belgium.be/fr/prevalence-des-pathologies-dans-les-etablissementspsychiatriques
Involuntary stays
| An involuntary admission, sometimes called a collocation, is intended as a protective measure. A patient can be ordered into involuntary admission by a magistrate if he or she is a danger to him or herself or to others. These patients are usually admitted to a PH. |  |
Evolution in the number of (continued) involuntary stays
|
|
The number of involuntary admissions has increased by 37.4% over the past 10 years[9]. |
More information about stays in PH and PDGH: https://www.health.belgium.be/
Patient flows
A psychiatric patient is not necessarily admitted to a hospital (PH or PDGH) in his or her region. For example, it is possible that a patient living in the Flemish Region is admitted to a hospital in the Brussels Capital Region. Hospitals that systematically attract a large number of patients from outside their area could have a greater need for hospital beds as a result.
Percentage of patient stays by patients’ place of residence and region of hospital in 2021
Most patients are hospitalised in a hospital within their region. In hospitals in the Flemish and Walloon regions, the figures are 97.4% and 95.6%, respectively. In hospitals in the Brussels Capital Region, 10.2% of patients come from the Flemish Region and 10% come from the Walloon Region. The place of residence is unknown for 11.5% of stays.
More information about patient flows: https://www.health.belgium.be/
[1]Source: FPS Public Health Central Institution File (CIC), situation at 01/01/2023.
[2]The public PH in Geel and Lierneux also have beds and places for ‘Family placement or psychiatric family care’ (index Tf). These are atypical of the Belgian hospital landscape and are not covered in this document.
[3]Source: STATBEL. Structure of the population, situation at 01/01/2023. Accessed on 01/10/2023, from https:// statbel.fgov.be/en/themes/population/structure-population
[4] This involved deducting the number of decommissioned beds from the number of accredited beds.
[5]Source: FPS Public Health Minimal Psychiatric Data (MPD); This concerned the number of accredited residential and partial stays in beds for adults (all code letters except K, k1, k2, Tf, Tfb, Tfp, Z and VP) in the year in question, regardless of the year of admission and regardless of whether the patient had already been discharged.
[6]The gender of the patient was unknown for 19 stays in 2021.
[7]For the sake of completeness, the category of 0-18 year olds is also stated. In exceptional cases, children and adolescents may be admitted to a psychiatric service for adults. Furthermore, stays in the 0-18 year old category may be the result of incorrect registration.
[8]Only partial and residential stays that had ended in 2021 were considered in this calculation.
[9] Source: FPS Public Health. Minimal psychiatric data (MPD); All new (ended and non-ended) stays for the year in question were selected (year stated = year of admission)
- Details
Care pathway for internees
 |
Internment is a legal security measure ordered by the criminal court for persons with mental illness who have committed a crime but who are deemed by the criminal court judges to have not been in control of their actions, and who also pose a danger to society. This internment measure under criminal law should not be confused with involuntary admission under civil law, whereby no crime has been committed.
|
It was standard practice for many years for internees to stay indefinitely in the psychiatric wards or society protection departments of correctional institutions. As the care provided in these institutions was inadequate, Belgium was regularly the subject of criticism by the European Committee for the Prevention of Torture and Inhuman or Degrading Treatment or Punishment. Ultimately, the Belgian State had numerous rulings pronounced on it by the European Court of Human Rights.
Under this pressure from within Europe, the governments invested in forensic care and the ‘Masterplans’, as they were known, came into being. The ‘Masterplan for Internment’ focuses on forensic psychiatric care. This stipulates that every internee is entitled to appropriate care.
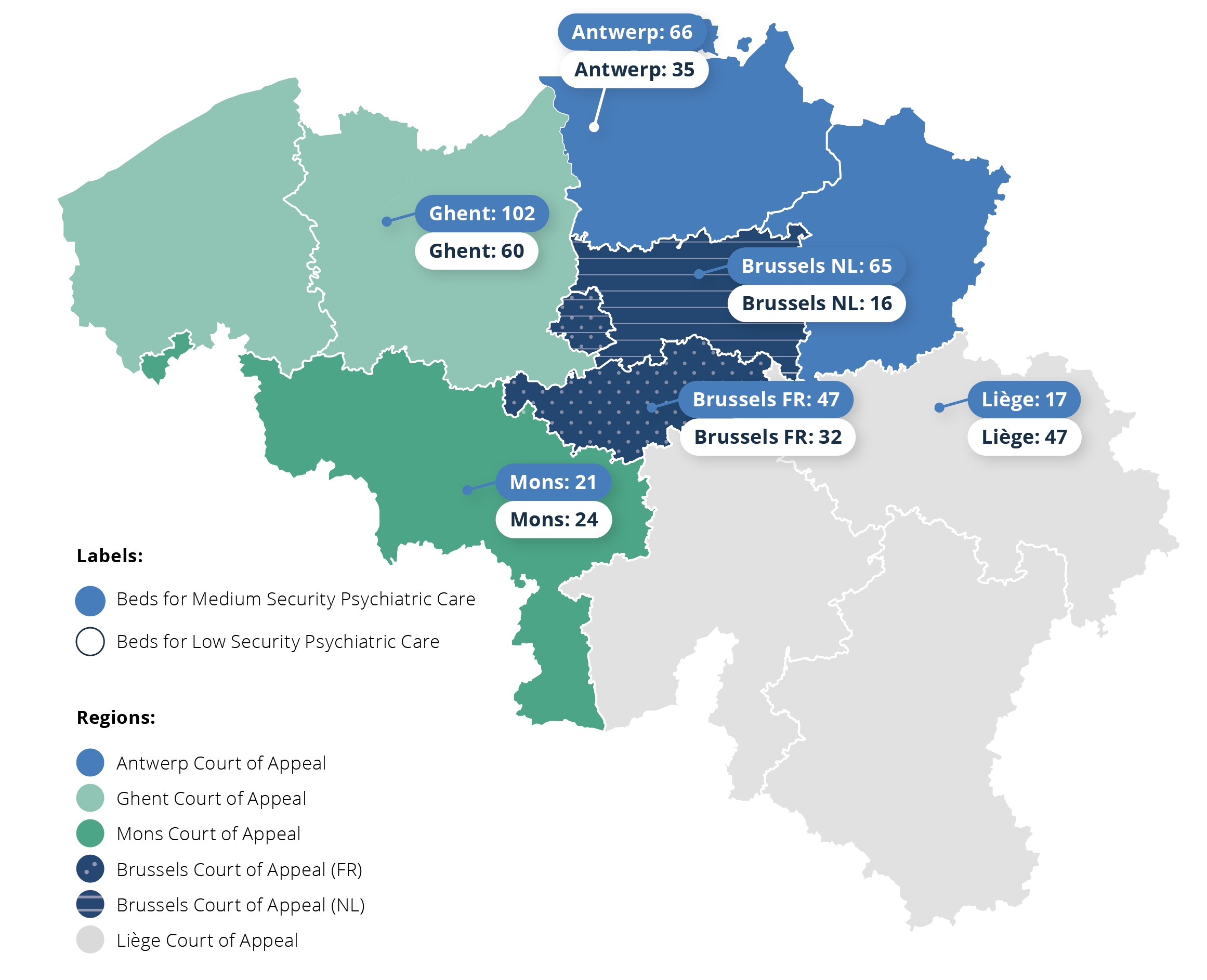
As part of mental health reform in 2014, a care pathway was developed for internees thanks to the launch of networks organised by the Court of Appeals (CoA). Network collaboration means that care providers and actors work together to realise personalised care pathways, based on the healthcare needs of patients.
The residential care offering for internees can be broadly divided by security level:
- High security care facilities provide care for internees with high risk profiles and high security needs;
- Medium security facilities/departments provide care for internees with moderate risk profiles and increased security needs;
- Low security facilities provide care for internees with low risk profiles and low security needs.

Number of crisis and time-out beds
Number of FTE for mobile and outpatient care for internees
Number of places for internees in PCH, SHI and alternative housing
Evolution in number of internees inside and outside prison
|
An average of 83% of internees stayed in a facility outside prison from 2018 to 2022. This equated to 3,263 people in 2022. Around one fifth of internees were placed in a Belgian prison. This equated to 486 people in 2018. This number rose to 850 by 2022[1]. This increase is mainly due to an increase in orders for internment. |
More information: https://www.internement.be/
Profile of the internees in a FPS health-funded care facility (excluding FPC)[2]
In 2020, there were 2,174 internees receiving treatment/support in a FPS Public Health-funded care service for this target group (excluding care capacity in forensic psychiatric centres (FPC)). These patients are cared for outside prison. The average age was 43.
Percentage of internees by age group
Top 3 most common offences among internees
|
More than one third of internees committed a violent crime against people, including beatings and wounding and unruly behaviour. Almost 20% committed a sexual offence and 13% were committed for a non-violent property offence. |
Top 5 most common diagnoses among internees
|
More than two thirds (78.6%) of internees had substance abuse problems. Other common diagnoses were psychoses (61.5%) and personality disorders (54.9%). In addition, over one third of involuntarily committed patients (36.2%) were also diagnosed with a mental disability. About 80% of the cases involved two or more comorbid disorders. |
[1]Source: Chamber of Society Protection
[2]Delannoy, D., Jeandarme, I., Pham, T., Pouls, C. (2023). Onderzoeksrapport Zorgtraject geïnterneerden [Research Report on Care Pathway for Involuntarily Committed Patients – 2020. Gent. Accessed 1 October 2023, from https://www.researchgate.net/publication/362889778_ Onderzoeksrapport_Zorgtraject_geinterneerden_-_2018; this refers to in FPS Public Health-funded care capacity (excluding Forensic Psychiatric Centres (FPC))
- Details
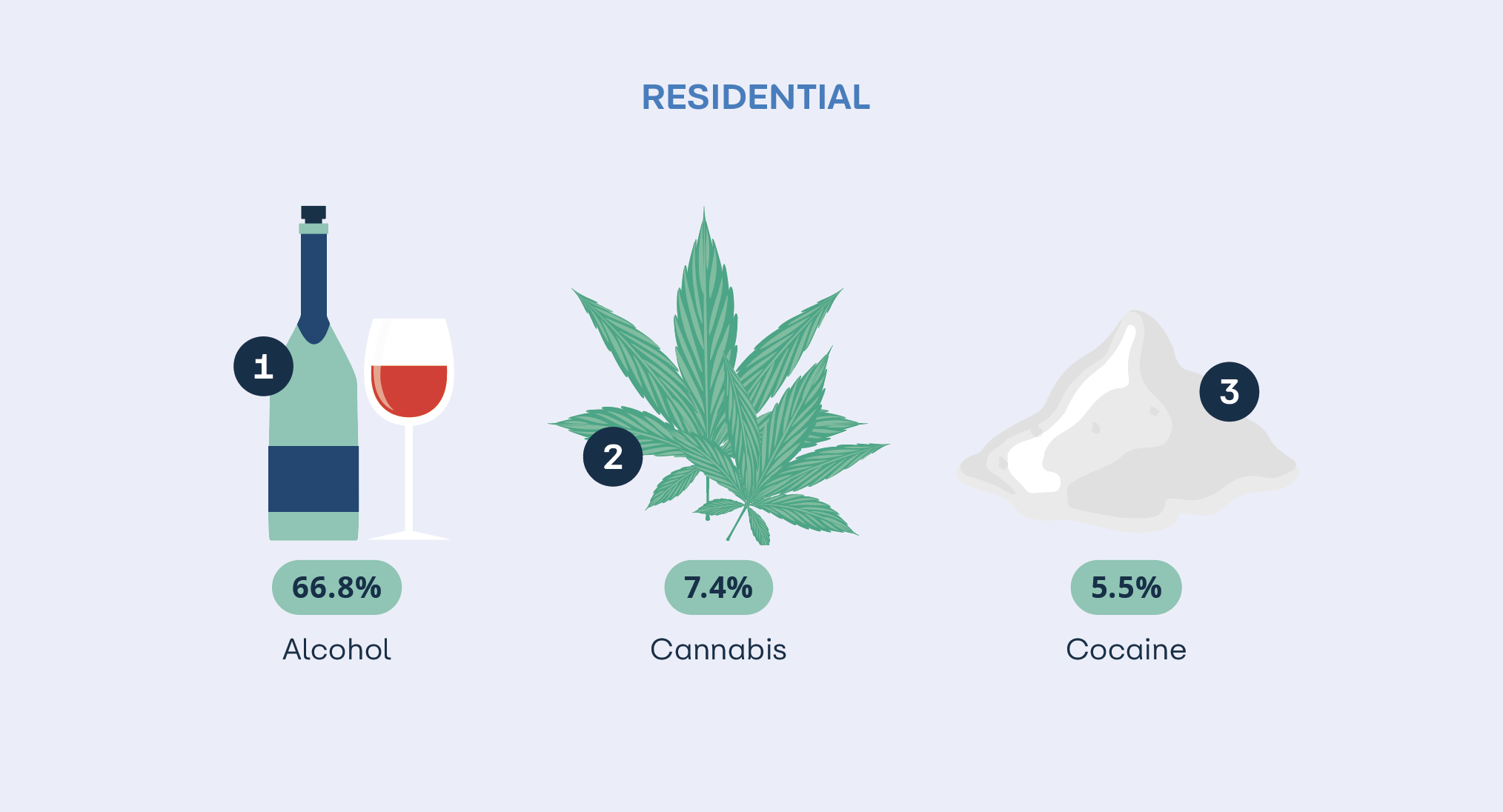
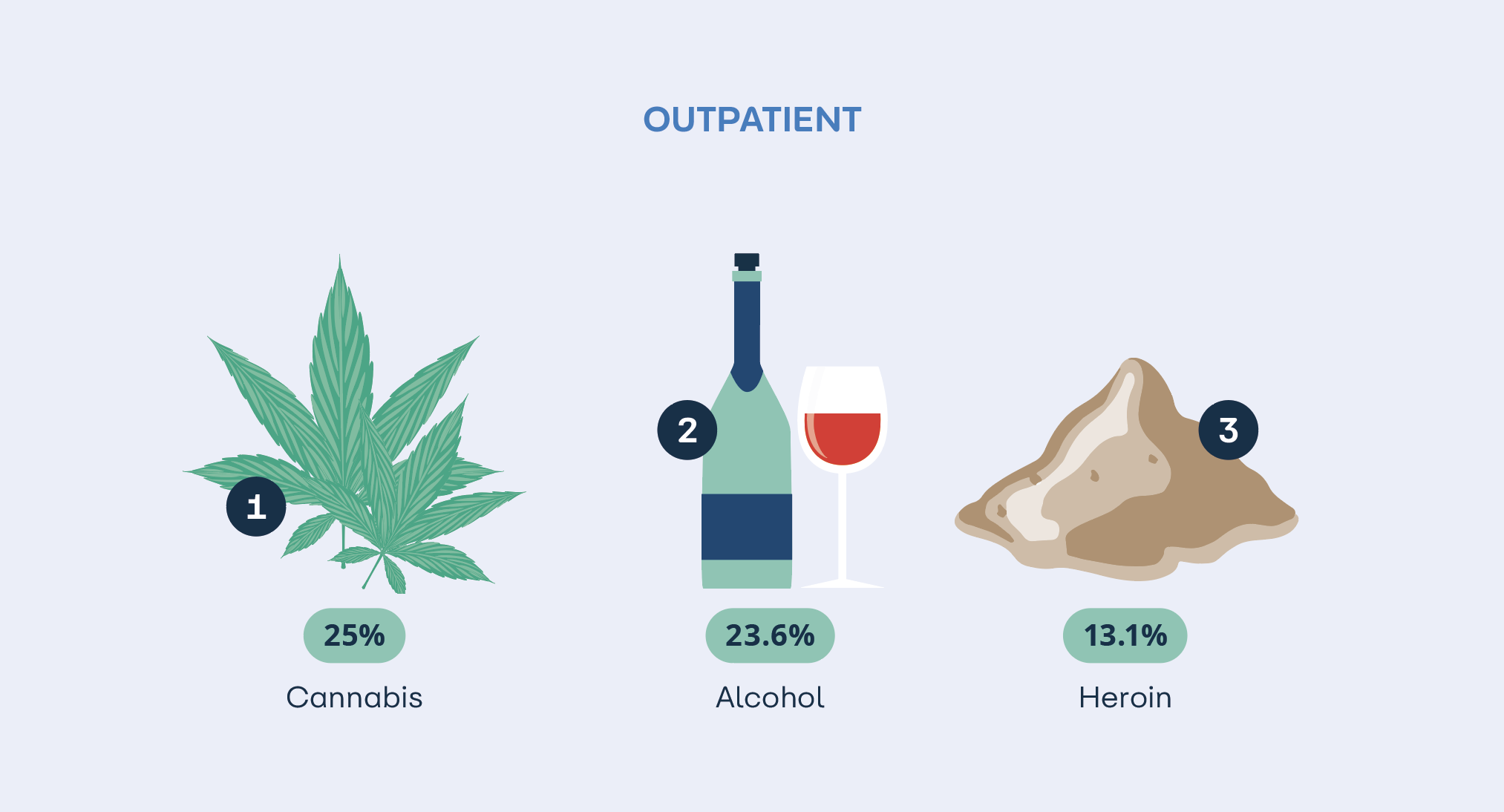
More than 26,000 new treatment episodes aimed at addressing substance abuse were recorded in 2021. This concerns the treatment of approximately 15,000 different individuals.
Two thirds of treatments (62.1%) took place in a residential context such as a psychiatric hospital, general hospital, crisis intervention centre or therapeutic community.
Number of treatment episodes in 2021 by facility type
Profile of patients:

The top three substances reported as the main substance differ according to the type of contact:
Learn more? Treatment Demand Indicator Register in Belgium | Sciensano.be