- Details
On March 30 2015, the Interministerial Conference on Public Health (IMC) approved the “Guide to a new mental healthcare policy for children and young people (MHCY)”. This drew the outlines of a comprehensive and integrated mental health policy for children and adolescents.
It is a comprehensive policy, on the one hand because it covers health promotion and prevention, to primary care and outpatient care, through to highly specialised residential care, and on the other hand, because it is intended for all children and adolescents aged 0 to 23 years. It is integrated because it seeks the seamless collaboration of facilities and providers from mental health, broader healthcare and societal aspects.
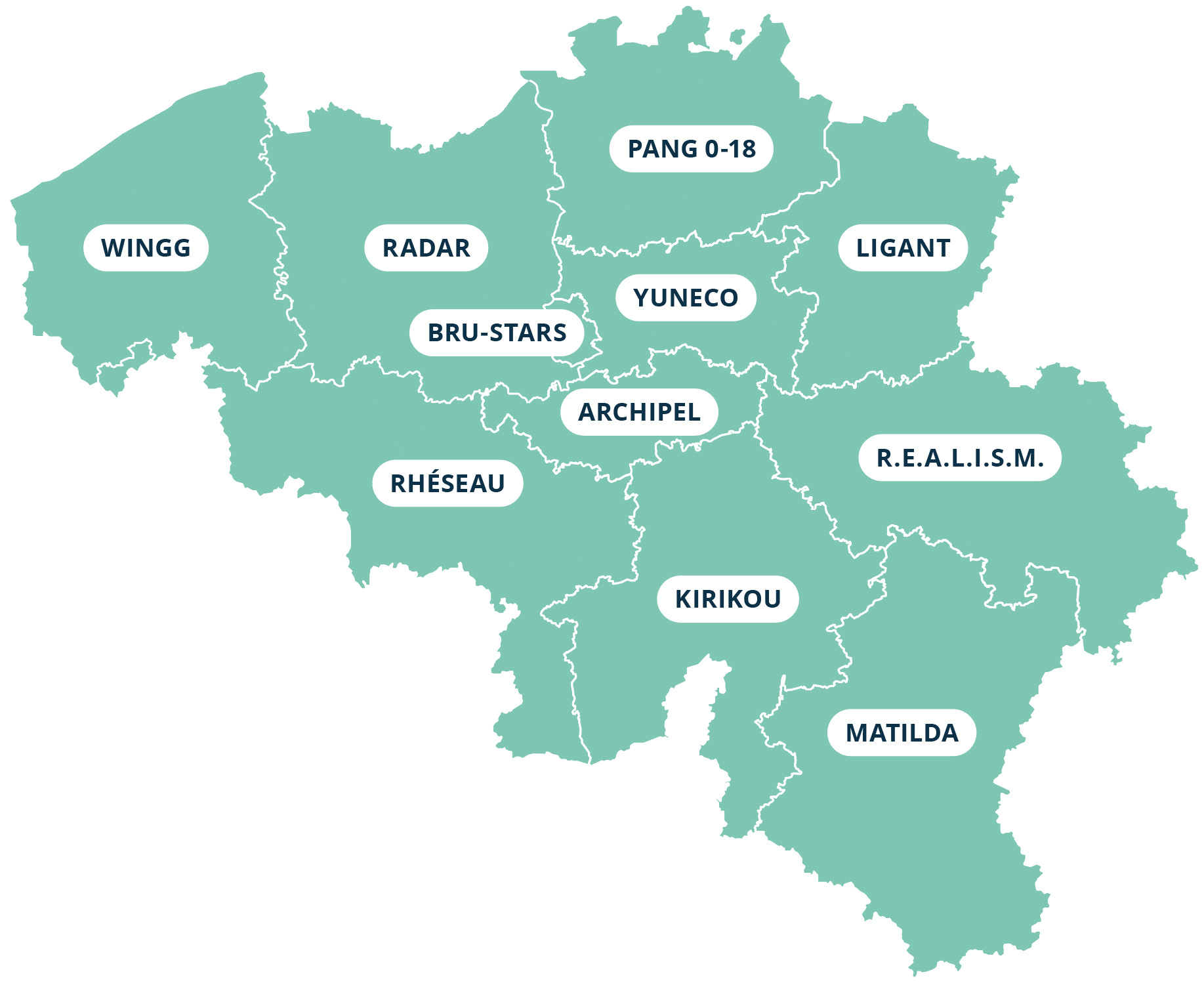
Eleven networks were set up almost immediately under the MHCY Guide, focusing on children, adolescents and young adults. The areas of operation of these networks correspond to the territories of the provinces and the Brussels-Capital Region[1].
The aim is to respond to the needs of these children and adolescents and their context or environment with the fastest and most continuous care possible. Each network consists of all the relevant actors, services, institutions, care providers, etc. of the sectors involved working together and coordinating their policies.
To optimise assistance, the MHCY networks are developing a number of programmes and modules funded by the federal government.
More specifically, it concerns:
- Programmes of crisis care and long-term care in which places for short-term care and acute treatment of adolescents in a non-life-threatening crisis situation with associated case management are provided in addition to a mobile offering.
- There is also investment in expertise and knowledge exchange between all actors involved regarding:
- individual children, adolescents and their context;
- specific sub-target groups of adolescents
- concerning all children and adolescents within the MHCY area of operation.
- We can then consider this to be an intersectoral consult and liaison programme and learning networks.
- In addition, dual diagnosis modules are being established in which customised care pathways are provided for children with intellectual disabilities combined with psychological problems, including crisis offerings and time-out options.
In addition, child and adolescent psychiatric hospital services, as well as forensic psychiatric units for adolescents, have also been strengthened with the addition of more staff. They not only contribute to the optimal operation of those services but also provide ‘bridging functions’ of care delivery and care transmission. This means that young patients are supervised even before their admission to a psychiatric hospital service and their departure is prepared from the start of admission.
To curb patient flow to these services, liaison teams are also deployed. They consist of psychiatrists, psychologists and psychiatric nurses, and provide counselling and care in non-psychiatric hospital services, e.g. paediatrics and emergency departments. They also provide support to caregivers in these non-psychiatric hospital services.
The MHCY networks are also given the means to realise innovative projects within cross-programme sites, ranging from additional forms of liaison where teams with psychiatric expertise provide care in non-psychiatric hospital services to the creation of pilot projects for adolescents in transition up to age 23.
More than 700 additional FTEs are being made available to the networks in order to realise all of these programmes, modules and projects.
Finally, the MHCY networks are driving the expansion of psychological care offerings in primary care for children and adolescents (see below).
[1] In the German-speaking Community, through a specific pilot project, a network is currently being created that will provide follow-up and care for all age-based target groups: children, adolescents, adults and the elderly.
- Details
Distribution of hospitals
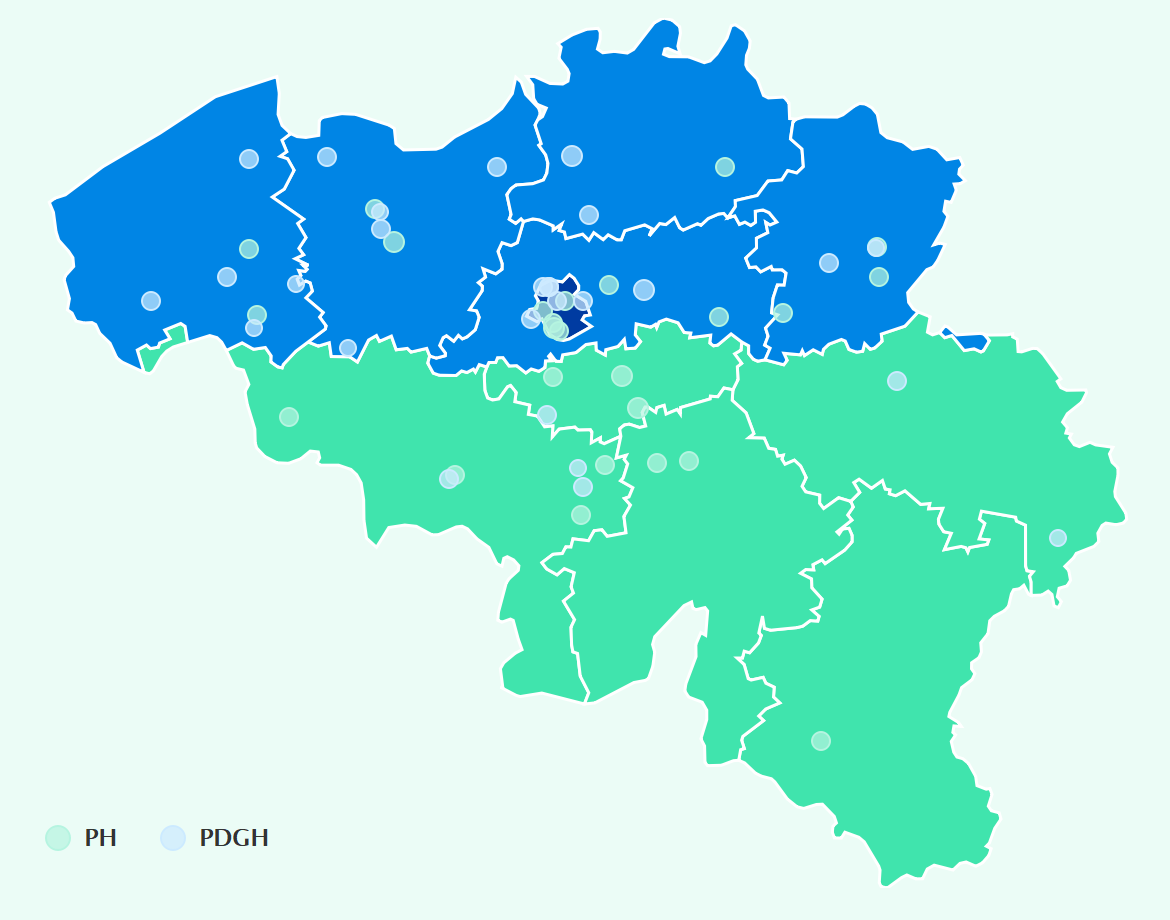
| A total of 52 hospitals, including 27 general hospitals with a psychiatric department (PDGH) and 25 psychiatric hospitals (PH) have a child and adolescent psychiatry service. | 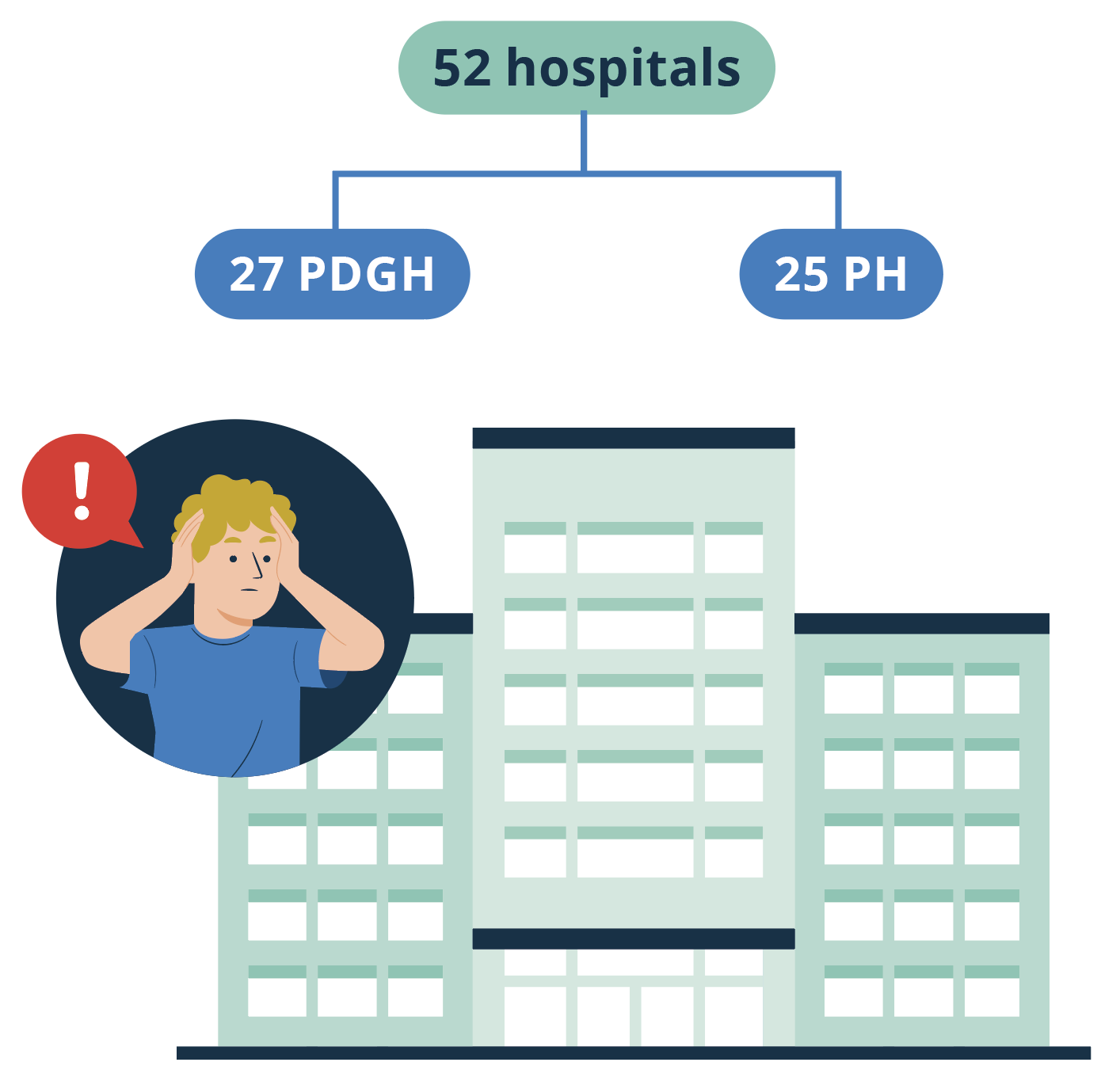 |
Number of hospitals according to number of accredited beds or places for adults with psychiatric problems 01/01/2023
The number of beds or places in these services is usually more limited compared with the services for adults. Notwithstanding the above, there is 1 PDGH with more than 100 beds or places. In contrast to the services for adults, psychiatric services for children and adolescents within PDGH and PH have a better balance in terms of the distribution of bed capacity.
Types of beds and places for residential and partial hospitalisation
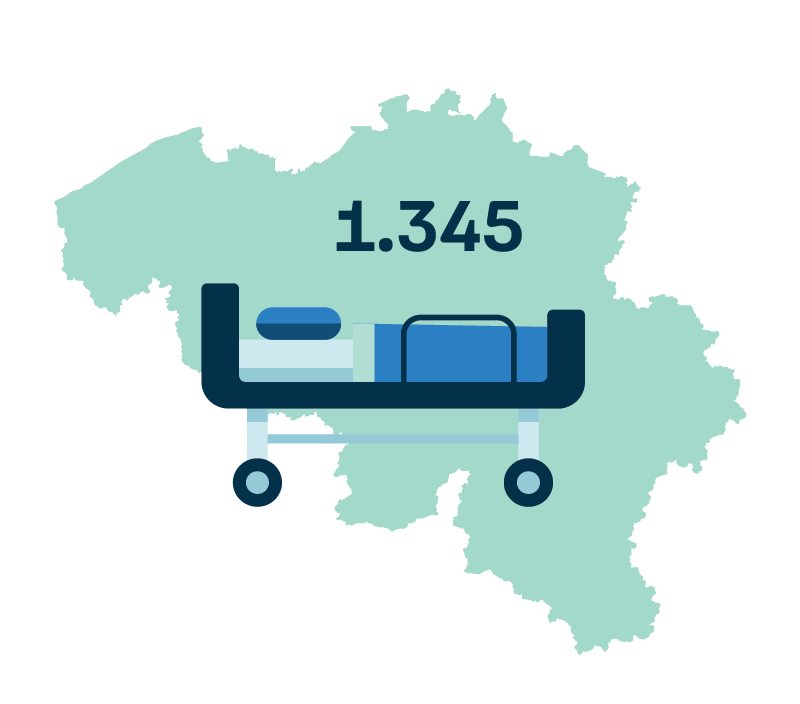 |
There were 1,345 beds and places in child and adolescent psychiatric services recognized in Belgium on 01/01/2023. This includes 711 beds for residential hospitalisation (index K), 555 places for day hospitalisation (index k1) and 79 beds for night hospitalisation (index k2). |
Number of accredited beds and places in child and adolescent psychiatric services on 01/01/2023
Number of accredited beds and places for children and young people per 100,000 inhabitants
|
The Brussels Capital Region, with 110 beds, has the most accredited beds per 100,000 inhabitants[1]. In the Flemish Region, 65 beds and places are accredited per 100,000 inhabitants, while this figure is 63 beds for the Walloon Region. |
The number of places for day hospitalisation (k1) for children and adolescents has tripled from 173 to 555 in the last 20 years. The number of accredited residential beds (K) and night hospitalisation beds (k2) remained stable.
Considered separately of political decisions in the past, this trend may indicate an increased need of care for children and adolescents with mental health problems, and especially a need for forms of (short-term) admission that are less severe than full hospitalisation. An adaptation of the programming standard would therefore not appear to be unjustified. Care for adolescents in particular merits special attention. However, under the current regulations, adolescents from the age of 15 can be admitted to adult psychiatric services in hospital. Even so, this target group is so specific that a solution within child and adolescent psychiatry should be prioritised. Experts recognise a transition age that can last up to the age of 23. However, for the purpose of designing programmes, only the number of children up to the age of 14 is taken into account.
Evolution in the total number of beds and places for children and adolescents
Characteristics of hospital stays
In 2021, there were 8,152 stays in PH and PDGH in child and adolescent psychiatric services[2]. The stays are evenly distributed across the institutions. The number of stays increased by 50.1% from 2007 to 2021. The largest increase was observed in PDGH (72.7% vs 33.6% in PH). We noted a decrease in the number of stays in 2020 due to the measures taken in the context of the COVID-19 pandemic.
Evolution in the number of hospital stays in psychiatric services for children and young people in PH and PDGH
Number of stays in child and adolescent psychiatry services by age group in 2021
| 57% of patients in child and adolescent psychiatric care in PH and PDGH in 2021 were female. More than half of the stays in these services were in the 13–17 age group (57%). Although adolescents older than 15 years can be admitted to adult psychiatry, a service for children and adolescents (K, k1 or k2) is still often preferred. In certain cases, a patient can still be admitted to a psychiatric service for children and adolescents even after their 18th birthday (11%). It is assumed that this transition age may continue to 23 years old. Nevertheless, in 2021, we still observe 145 stays by people older than 24 years (2%). |
Evolution in the number of stays in child and adolescent psychiatry services by age group
|
|
In the period from 2007 to 2021, we see that the number of stays by children aged 0 to 3 tripled. The stays by children and adolescents in the 13-17 age group increased by more than half. The number of 18 to 23-year-olds staying in child and adolescent psychiatric services decreased by 5.7%. |
Evolution in the number of stays in PH and PDGH by type of hospitalisation
|
|
The last 15 years have seen an increase in all forms of stays in child and adolescent psychiatric hospital services. We have observed an increase of 39.1% in the number of residential stays and almost a doubling in the number of day hospitalisations (k1), where the child or adolescent stays at home at night and on weekends. There are few stays (87 in 2021) in which the child or adolescent stays in the hospital only in the evening and at night (k2). |
Duration of stay in psychiatric services for children and adolescents in PH and PDGH in 2021
|
|
Around 80% of stays in a child and adolescent psychiatric service in PH and PDGH last less than 3 months. |
Duration of stay in psychiatric services for children and adults in PH and PDGH in 2021
|
|
From 2007 to 2021, we saw an increase in the total number of inpatient days for residential hospitalisation (8.7%). For day hospitalisation, the number of stays more than doubled (151%). Due to increased pressures in child and adolescent psychiatric services, it was decided in 2021 to increase staffing levels for these services and to create liaison teams to supervise and treat adolescents with mental health problems admitted to non-psychiatric hospital services. |
| Based on the primary diagnosis given to patients in PH and PDGH in the psychiatric wards for children and adolescents, we can see the following top 3 diagnoses in 2021: adjustment disorders, autism spectrum disorder and depressive disorders. Stays with one of these 3 main diagnoses represent 44.3% and 48.5% of all stays in PH and PDGH, respectively. |  |
Top 10 main diagnoses in 2021
More information about diagnoses made during admission to PH or PDGH: https://www.health.belgium.be/
Patient flows
As is the case with stays in adult psychiatry services, patients in child and adolescent psychiatry services are not necessarily admitted to a PH or PDGH in their own region.
In hospitals in the Flemish and Walloon regions, 95.6% and 92.1% of patients respectively are domiciled in the same region. Only half of the patients from the Brussels Capital Region are admitted to hospitals there. Almost one fifth of patients there are from the Flemish Region and 27.1% are from the Walloon Region.
Percentage of patient stays by patients’ place of residence and region of hospital in 2021
More information about patient flows: https://www.health.belgium.be/
[1]Source: STATBEL. Structure of the population, situation at 01/01/2023. Accessed on 01/10/2023, from https://statbel.fgov.be/fr/themes/population/structure-de-la-population; only the number of inhabitants below the age of 15 were taken into account.
[2]Source: FPS Public Health, Minimal Psychiatric Data (MPD). This is the number of accredited residential and partial stays in beds for children (index K, k1, k2) in the relevant year, regardless of the year of admission and regardless of whether the patient had already been discharged.