- Details
When a citizen calls 112 to ask for medical assistance, a process is initiated in which several actors play a role. These actors are discussed in detail later on.
112 Emergency centres
General operation
There are 10 emergency centres for 112 calls in Belgium: one in each provincial capital, with the exception of Walloon Brabant, and one in the Brussels-Capital Region. The calls from Walloon Brabant are handled by the Hainaut 112 emergency centre.
 “Belgium has 10 emergency centres for 112 calls.”
“Belgium has 10 emergency centres for 112 calls.”
Via the 112 emergency number, a person requesting emergency assistance in Belgium is referred to one of the 10 emergency centres. In 2023, the 112 emergency centres were manned by 447 operators[1]. An operator at the emergency centre will answer the call and analyse the request for assistance. Using the Belgian Medical Regulation Manual, which consists of established protocols, the 112 emergency centre operator classifies the request for assistance according to its a severity level. The mostappropriate resources are then dispatched. This may be an ambulance, a Paramedical Intervention Team (PIT) or a Mobile Emergency Group (MUG/SMUR).
The operators are assisted by a medical director[2], a deputy medical director [3] and nurse regulators[4].
- The medical director is responsible for supervising the medical quality of the emergency assistance. They must have a qualification as an emergency doctor.
- The deputy medical director holds the special professional title of nurse specialised in intensive and emergency care. Under the coordination of the medical director, they perform tasks within the 112 emergency centre as a functional medical authority and project officer, and act as a link between the various partners of the 112 emergency centre.
- The nurse regulator supports and advises the operators by offering them, among other things, appropriate medical training. The nurse holds the special professional title of emergency nurse. They should also have specific training in crisis management and contingency planning.
Non-urgent medical assistance via a call to 1733
1733 is a central number intended to provide non-urgent medical services to citizens outside of business hours such as on week nights, weekends or public holidays. This number is linked to the local on-call medical services. Operators at some 112 emergency centres already handle calls to the 1733 number.
 |
“The 1733 number can be used in 1,109 locations to reach an on-call GP.” |
As of 4 January 2024, the inhabitants of 1,109 locations, identified by postcode, can contact an on-call GP using the 1733 number[5].
In 602 of the 1,109 locations, 1733 calls are handled by a 112 emergency centre. This is the case for locations that are covered by the 112 emergency centres in Arlon, Antwerp, Mons, Bruges, Leuven or Liège. Which emergency centre takes the call depends on where the 1733 call originates. The call handling is organised in a complementary way and in synergy with the 112 call system. Trained operators refer the person requesting care to the most suitable care offer on the basis of the Belgian Medical Regulation Manual.
In the 507 other locations, calls are currently transferred directly to an on-call medical staff member or an on-call GP. Due to the acute shortage of operators, it is not yet possible to have the 112 emergency centre answering all 1733 calls in all municipalities.
To find out more about the 1733 number:
www.1733.be
Taskforce operators: when operators are in short supply
Despite the constant efforts used to strengthen the numbers in the 112 emergency centres, there are still not enough operators. It is estimated that a 112 emergency centre needs at least three operators to function well. Only once the centre has four or more operators does it have sufficient capacity to handle 1733 calls. In late 2023, the Directorate General for Civil Security of the FPS Home Affairs, working with its partners, including the FPS Public Health carried out a 360-degree exercise designed to tackle the difficulties encountered in the 112 emergency centres. This partnership resulted in the creation of a master plan for the 112 emergency centres. This plan is structured around seven major issues: governance (1), organisation of work (2), human resources (3), tools and technology (4), well-being (5), communication (6) and funding (7). The action plan contains nearly 150 actions and presents levers to improve the current situation significantly.
The solutions identified included the creation of an accelerated recruitment procedure, known as the “Fast Lane”. In just one day, the candidate sits all the exams and attends the interviews that form the selection process. The training pathway has also been adapted so that future operators can handle 1733 calls during their training to deal with 112 calls. This win-win situation benefits both the operators, who gain hands-on experience in their future role before they finish their training, and the 112 emergency centre that has staff who are available to relieve the 112 operators more quickly.
At 15 March 2024, 32 operators were already in place and, via the Fast Lane, 25 individuals had accepted a position as a 112 or 1733 operator. 31 positions were still open. As a comparison, 32 112 and 1733 operators were recruited in 2023.
A second solution which was proposed involved creating two virtual, supra-provincial emergency centres (one Dutch-speaking and one French-speaking) for the 1733 number. The operators who will work in this virtual 1733 centre will continue to work physically from the stations in the 112 emergency centres in the different provinces. However, 1733 calls that end up in this virtual centre will be handled by operators regardless of which competent 112 emergency centre on the ground should have handled the call. Previously, a call made in the Province of Hainaut was handled by the Mons 112 emergency centre. Using this system, the same 1733 call may be handled by an operator at the Liège 112 emergency centre, for example. Given that the handling of calls no longer depends on where the operator works but their availability, this scheme could be used to resolve the problems related to staff shortages. In other words, it would enable the operator who handles 1733 calls in the Leuven emergency centre to take a 1733 call made by a caller in the city of Antwerp in the event that the 1733 operator in the Antwerp emergency centre is already on a call with another caller. Previously, this type of call would be put on hold until the operator at the Antwerp emergency centre finished their initial call. The pooling of human resources in emergency centres with the same linguistic role should lead to better management of 1733 calls.
The French-speaking virtual supra-provincial centre for 1733 was opened on 1 April 2024. After a test phase, the on-call medical staff were gradually integrated every 15 days. The Dutch-speaking virtual centre followed a month later on May 1st 2024. Eventually, all of Belgium should be covered.
Ambulance services and on-call rotations
In Belgium, as of 1 January 2024, 116 organisations had signed an “Ambulance service for emergency medical assistance” agreement with FPS Public Health. In this agreement, services commit to being available at agreed times.
|
The following organisations are involved in providing emergency medical assistance:
|
Only services that have concluded a formalised, signed agreement can be dispatched by a 112 emergency centre. Having such an agreement is also a condition for obtaining a grant from the FPS Public Health. Services that have not signed an agreement handle non-urgent patient transport, provided that they are approved by the federated entities.
Based on the agreement, one or more on-call rotations are each manned by two paramedics, who are ready to go to a patient at the emergency centre’s request. On 1 February, in Belgium, there were 420 on-call staff for both an ambulance (379) and a Paramedical Intervention Team (41)[6]. Some on-call rotations are set to begin during the year. By the end of 2024, Belgium will have a total of 441 on-call rotations funded due to the integration of 3 on-call ambulances and 18 additional on-call PIT.
- Most on-call rotations have an on-call service where the paramedics are on duty at the departure point. These on-call services have a rest area. This is also known as an ‘accommodated’ on-call rotation. This is the most frequently-used on-call model (345 stations).
- A number of on-call rotations have an on-call service where the paramedics are on duty at home and go to the departure point in the event of a call. This is known as an ‘unaccommodated’ on-call rotation. This type of on-call rotation is the least common model (26 posts).
- Some on-call rotations offer a “mixed” on-call service, combining accommodated and unaccommodated on-call rotations. A total of 49 posts are organised using this model.
Learn more about ambulance services:
https://www.health.belgium.be/
Number of on-call rotations for ambulance and PIT by type (01/02/2024)
The various emergency services for emergency assistance
In a situation where there is a need for emergency medical assistance, various resources can be dispatched to the location of the emergency, i.e. an ambulance, a Paramedical Intervention Team (PIT) or a Mobile Emergency Group (MUG/SMUR). On the basis of protocols established in the Belgian Medical Regulation Manual, the operator from the emergency centre determines which resource will be activated. In addition, based on the above protocols, an operator may refer the caller to an on-call general practitioner.
Ambulance
An ambulance is a vehicle that has been specially adapted, furnished and equipped to provide basic life support at an intervention site on the one hand, and on the other hand to safely transport a patient to hospital. An ambulance has the necessary equipment for monitoring and providing first aid. There are at least two paramedics in each ambulance. They are usually the first health workers to arrive at the intervention site.
In Belgium, there are 379 on-call rotations for dispatching ambulances approved for emergency medical assistance. Of these, 31 are located in the Brussels-Capital Region, 201 in the Flemish Region and 147 in the Walloon Region. Considering the number of on-call rotations per 100,000 residents, there is a greater presence of on-call rotations in the Walloon Region (3.98 per 100,000 residents), compared to 2.95 and 2.49 per 100,000 residents in the Flemish and Brussels-Capital Regions respectively.
Intermediate ambulance
An intermediate ambulance is an ambulance that is mostly designed for non-urgent medical and health transport but which can be integrated into emergency medical assistance on an ad hoc basis in the event of a disaster or crisis or as a temporary substitution vehicle for an existing 112 dispatch. This system should allow emergency medical assistance to be scaled up quickly when needed.
Non-urgent patient transport by ambulance is a regional competence. For example, this may involve the transfer of a patient between two hospitals or an examination at the hospital of a patient on a stretcher. The intermediate ambulance must be approved by the federated entities to be able to carry out non-urgent medical and health transport but also by the FPS Public Health so that it can be integrated into emergency medical assistance. Until 2024, this type of resource was a grey area midway between the competences of the federated and federal entities. A close partnership between the federal state and the federated entities has clarified the use of intermediate ambulances and their defining criteria.
Paramedical Intervention Team (PIT)
The Paramedical Intervention Team (PIT) is a team that intervenes in more serious cases. The team consists of at least one paramedic and one nurse who holds the special title of intensive and emergency care. A PIT ambulance can be dispatched for interventions where the care can be assigned to a nurse. In addition, a PIT is sent in some cases when no MUG/SMUR is available.
In addition to the basic equipment for an ambulance, a PIT ambulance must have the necessary equipment to carry out all its missions. Indeed, more tasks are assigned to the nurse and the paramedic using standing orders (see chapter Quality and Innovation). This allows the nurse to perform some medical acts on site. Furthermore, the PIT team can contact a referring doctor if medical guidance is necessary. This is a doctor who remotely advises and guides the nurse through the use of the standing orders.
The PIT function is currently a pilot project. In October 2009, 24 pilot projects in the framework of a PIT function were launched in Belgium. Currently, no new services are being launched within the pilot project, but several hospitals are taking the initiative to upgrade an existing, accredited ambulance service to a PIT function themselves. By the end of 2024, 27 new PIT functions will integrate emergency medical assistance as part of the urgent inter-hospital transport PIT project via hospital network. This will bring the total number of PIT functions in Belgium to 51. A PIT function may have several paramedical intervention teams.
At 1 February 2024, there were 41 on-call rotations held by a paramedical intervention team (PIT) in Belgium, 25 in the Flemish Region, 13 in the Walloon Region and 3 in the Brussels-Capital Region.
However, if the number of PIT on-call rotations per 100,000, residents is considered, it can be seen that these numbers are almost the same in Flanders and Wallonia. There are 0.35 PIT on-call rotations per 100,000 inhabitants in the Walloon Region compared with 0.37 in the Flemish Region. In the Brussels-Capital Region, there are 0.24 PIT on-call rotations per 100,000 inhabitants.
Mobile Emergency Group (MUG/SMUR)
A Mobile Emergency Group (MUG/SMUR) is a mobile medical team that provides advanced life support during an intervention in the context of an emergency situation. The team consists of at least one emergency doctor and one nurse who holds the special title in intensive and emergency care. The MUG/ SMUR station is located near a hospital.
The MUG/SMUR team is always accompanied by an ambulance at the intervention site and can be dispatched at the request of the operator at the 112 emergency centre or at the request of the on-site ambulance crews if they feel that a doctor is required.
At 1 February 2024, there were 94 MUG/SMUR functions in Belgium, 49 in the Flemish Region, 36 in the Walloon Region and 9 in the Brussels-Capital Region. Two of these 94 MUG/SMUR functions concern MUG/ SMUR helicopters based in the Province of Liège and in Bruges, which are currently being evaluated as pilot projects.
Considering the number of MUG/SMUR functions per 100,000 residents, there is a greater presence of MUG/SMUR functions in the Walloon Region (0.97 per 100,000 residents), compared to 0.72 per 100,000 residents in the Flemish and Brussels-Capital Regions. The greater presence of MUG/SMUR in the Walloon Region can be explained by the more sparsely populated areas, which require a greater presence of MUG/SMUR functions to ensure rapid care. The aim is to achieve equal access to emergency assistance in the various regions of the country. To this end, the number of MUG/SMURs is determined by programming criteria that includes the population of each province. These criteria were defined in a Royal Decree.[7]
Number of on-call rotations for accredited ambulances and PIT and MUG/SMUR
functions per 100,000 inhabitants by region
Learn more about the location of the MUG/SMUR and PIT functions
and the departure locations for ambulances:
https://www.health.belgium.be
Emergency services
| Typically, an ambulance will transport the patient to the nearest hospital with a specialist emergency care service, as determined by the 112 emergency call centre. |  |
|
The nearest hospital is calculated in line with the journey time and not in line with the number of kilometres: e.g. the distance from Egenhoven via N264 to UZ Leuven campus Gasthuisberg is 5 km, but the journey time is 9 minutes. The distance from Egenhoven to Heilig Hart Regional Hospital is 4.2 km, but the journey time is 10 minutes. In this case, then, the patient will be taken to UZ Leuven campus Gasthuisberg even though the Heilig Hart Regional Hospital is closer, because the journey time is shorter. When a MUG/SMUR intervenes, the doctor can deviate from the fastest journey time provided that this is based on the diagnosis of the patient or the need for a specific therapeutic platform (neurosurgery or neonatology, for example). |
In Belgium, we have two types of emergency services:
- A specialist emergency care service: this service must be permanently staffed by an emergency doctor and a minimum of two nurses, at least one of whom must have obtained the special professional title in intensive and emergency care. This service must be able to stabilise and restore a patient’s vital signs. 112 ambulances must be directed to this type of service to drop off a patient.
- An emergency first responder service: each critical hospital that does not have a specialist emergency care service must have an emergency first responder service. One nurse and one doctor on duty for the entire hospital are sufficient.
At 1 February 2024, there were 124 emergency departments in Belgium, spread across several hospital campuses[8]. Of these, 2 campuses in the Flemish Region, 2 campuses in the Walloon Region and 1 in the Brussels-Capital Region only have an emergency first responder service. The others are specialist emergency care services.
Staff at the various emergency services for emergency assistance
Nurses and paramedics licensed to work in emergency medical assistance can be identified through a badge issued by the FPS Public Health.
- Paramedics can be issued this badge by obtaining a paramedics licence. This licence is obtained upon successful completion of the training organised by the provincial training centres.
- For nurses holding a special professional title of emergency and intensive care, obtaining a badge from the FPS Public Health does not require any additional training. For other nurses wanting to work in emergency medical assistance, the badge can be obtained by successfully completing the training in the provincial training centres.
- For doctors, no badge is required to work in a MUG/SMUR.
Number of care providers by type with licence and badge (31/12/2023)[9]
It should be noted that the number of nurses specialising in intensive and emergency care with licence and badge has almost doubled in the last ten years.
Change in the number of care providers by type with licence and badge
To find out more about paramedic training:
http://www.ejustice.just.fgov.be/eli/arrete/2024/01/01/2023048632/moniteur
[1]Source: FPS Home Affairs and the Firefighting and Emergency Medical Assistance service of the Brussels-Capital Region.
[2]The duties of the medical director are laid down in the Royal Decree defining the function, tasks and competence profile of the medical director of 112 centres.
[3]The duties of the deputy medical director are laid down in the Royal Decree defining the function, tasks and competence profile of the deputy medical director of 112 centres.
[4]The duties of the nurse regulator are laid down in the Royal Decree defining the function, tasks and competence profile of the nurse regulator.
[5]In other municipalities, the on-call GP can be reached using a local phone number.
[6]On-call rotations as discussed above are only organised for ambulances and Paramedical Intervention Teams (PIT). For this reason, no data on the MUG/SMUR functions has been incorporated here.
[7]Royal Decree of 20 September 2002 determining the details of the maximum number and the programming criteria applicable to the “Mobile Emergency Group” function.
[8]Source: FPS Public Health (2024, 1 February). Hospital Infrastructure Repository (HIR). [Dataset]
[9]Source: FPS Public Health (31 December 2023). E-CAD. [Dataset]
- Details
The relief operation for a collective emergency situation or major federal crisis is coordinated from the National Crisis Centre, which is part of the FPS Home Affairs. However, the principles of management developed at a federal level are also applied at a provincial and municipal level for incidents of lesser importance.
Five disciplines
|
A disaster or collective emergency situation is tackled by various intervention services, whereby each discipline has a mono-disciplinary intervention plan that describes its own operation. Where multiple disciplines are deployed simultaneously, joint coordination is required, this is referred to as a multi-disciplinary deployment.[1] |
|
“ 5 disciplines or intervention services can be called upon in the event of a disaster or crisis.“ |
|
Discipline 1: emergency rescue zones
|
| Discipline 2: medical, sanitary and psychosocial services Discipline 2 missions are performed by medical and psychosocial services (e.g. ambulance services, MUG/SMUR services, the Red Cross, psychosocial workers, the Federal Health Inspectorate, etc.). The most important missions in this discipline are discussed later on in this report. |
|
Discipline 3: police at the scene of the emergency
|
|
Discipline 4: logistical support
|
|
Discipline 5: information to citizens
|
Emergency planning
The purpose of emergency planning is to anticipate a disaster or crisis. A whole range of measures, procedures, tools and coordination mechanisms are put in place. In this way, the resources (both human and equipment) needed to manage the situation can be deployed quickly and efficiently. Depending on the nature of the incident, there are several different contingency plans.
- Multi-disciplinary emergency plans are developed by different authorities. These emergency plans are intended for crisis management at a federal, provincial or municipal level. For example, this type of contingency plan was used during the terrorist attacks in Zaventem and Maelbeek and the COVID-19 crisis;
- Mono-disciplinary intervention plans: these plans aim to develop the missions per discipline, so a discipline can start independently and act quickly. In addition, an emergency plan makes it possible to cooperate with other disciplines;
- Internal emergency plans: these are plans drawn up at the level of an institution, e.g. a hospital.
To find out more about emergency plans:
National Crisis Centre - Contingency Plans
Below, we will examine the mono-disciplinary contingency plan for medical, sanitary and psychosocial assistance (discipline 2), for which the FPS Public Health is responsible in an emergency situation.
This emergency plan describes the following missions:
- Initiating the medical chain;
- Administering medical and psychosocial care to victims and people involved in the emergency situation;
- Organising the transport of victims;
- Taking measures to protect public health.
|
The Federal Health Inspector plays an important role in executing this contingency plan. This individual is the local representative of the FPS Public Health in relation to emergency medical assistance. They are in direct contact with the governor, the mayor, health professionals and citizens. The Federal Health Inspector is assisted by an expert incident and crisis manager (ICM), a psychosocial manager (PSM) and a 112 medical team. This team consists of a medical director, a deputy medical director and nurse regulators (see ‘Organisation’ section) for each 112 emergency centre. Together, they form a ‘Federal Health Inspectorate Cluster’. The clusters are tasked with the following:
|
To find out more:
https://www.health.belgium.be
Three specific sub-plans that were developed as part of the above missions will now be discussed.
|
Medical care |
Psychological Care |
Public health |
||
| The Medical Contingency | The Psychosocial |
Risks and Demonstrations Plan |
||
| Plan | Intervention Plan | |||
| MIP |
PSIP |
RDP |
The Medical Contingency Plan (MIP)
The first emergency services (police, ambulance service or fire brigade) on the scene can request the activation of a medical contingency plan (MIP)[2]. Only a few professionals are authorised to activate a MIP, namely:
- the (deputy) medical director[3] ;
- the first MUG/SMUR doctor at the scene;
- a federal health inspector;
- an incident and crisis management (ICM) expert;
- Head of the Response Service of the Directorate-General for Health Emergency Preparedness and Response of the FPS Public Health.
The emergency centre with territorial jurisdiction will formally declare the MIP.
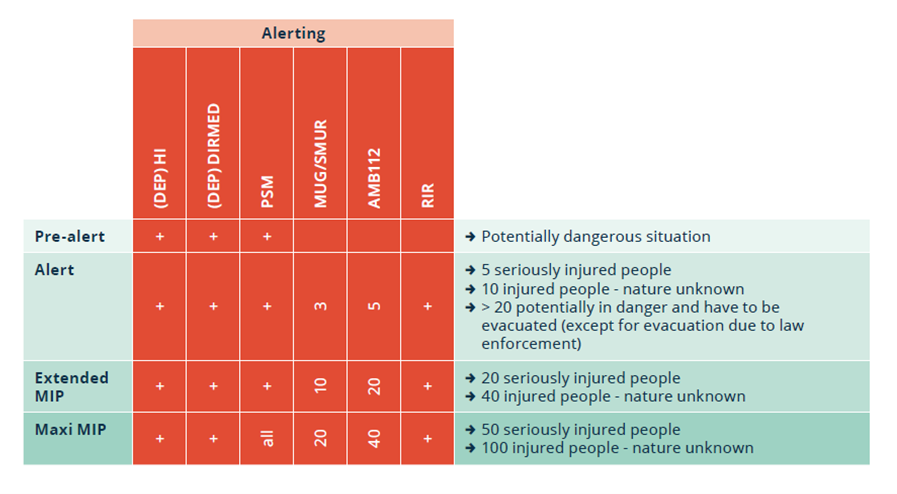
An MIP has different levels, with an increasing use of resources depending on the phase the MIP has reached. The (deputy) health inspector ((DEP)HI), (deputy) medical director ((DEP)DIRMED) and psychosocial manager (PSM) are always called. Depending on the phase, the Medical Emergency Group (MUG/SMUR), ambulances (AMB 112) and rapid intervention resources (RIR) are deployed.
The scaling up and down of plans is carried out by the 112 emergency centre on the basis of the information obtained from the people referred to above. When an MIP is scaled up, the 112 emergency centre in the affected province can call upon the resources of neighbouring provinces.
The Federal Minister of Public Health has an agreement with the Belgian Red Cross to provide support in the event of a (medical) emergency. This includes, among other things, providing the following:
- Ambulances and paramedics.
- Rapid Intervention Resources (RIR) for the establishment of the advanced medical post.
- Liaison officers: these are people who establish contact during an emergency and ensure communication between the various partners involved.
- Logistical support (sanitary kits, camp beds, blankets, etc.).
- A deployment of “Emergency Social Intervention”: these are volunteers who provide emergency psychosocial support in large-scale relief operations during disasters or severe cases.
The Head of the Response Service of Directorate-General for Health Emergency Preparedness and Response, the federal health inspectors and the incident and crisis management expert coordinate emergency medical assistance during a crisis. When the crisis is of such a magnitude that major socio-economic consequences are feared, administrative control (mayor, governor) is also required.
| For example, during a large industrial fire, a toxic cloud moves towards surrounding businesses. At that point, a decision must be made on whether to evacuate the factory for health reasons. This decision is made by the director of the operational command post or, in the administrative phase, by the mayor or governor. This decision has financial implications. Compensation may also need to be paid. The various disciplines have an advisory role at the municipal or provincial coordination centre (CC) at that point. |
The Psychosocial Intervention Plan (PSIP)
A collective emergency could cause serious psychosocial harm to a large number of people. As a result, there may be a need for appropriate assistance for those directly involved and their loved ones. In order to address this need, a Psychosocial Manager (PSM) works alongside the Federal Health Inspector (FHI). The actions within psychosocial support are aimed at stimulating the resilience of those affected and are targeted at both the direct and indirect victims of the emergency situation. The federal government is responsible for psychosocial assistance in the acute phase. Psychosocial support in the aftermath of a disaster is a task for the communities.
|
The following basic tasks of a psychosocial manager are to be carried out in the acute phase of an emergency situation:
|
| For example, during a fire at an assisted living facility, the family needs information about their family member. The psychosocial manager concerned will organise an information point at a nearby sports hall. |
To find out more about the PSIP:
www.health.belgium.be
Risks and Demonstrations Plan (RDP)
When a large-scale activity is organised, it may be necessary to provide a medical aid station as a precautionary measure. Using the Risks and Demonstrations Plan (RDP) questionnaire, the federal health inspectors give advice based on a risk analysis. The competent authority (the mayor or governor concerned) is advised on the necessary medical resources.
International emergency assistance
When there is a disaster or incident abroad, one of the FPS Public Health’s missions is to provide aid and assistance to the affected country if it officially requests it. Below we have opted to focus on two projects that illustrate the international action of the FPS Public Health.
Belgian First Aid and Support Team
The Belgian First Aid and Support Team (B-FAST) is an inter-departmental federal structure that deploys Belgian emergency assistance abroad.
The FPS Public Health, which works with the Ministry of Defence, the FPS Home Affairs and the FPS Foreign Affairs under the B-FAST mission, is responsible for the operational maintenance of the following modules:
- A water purification system module that includes the storage and distribution of purified water.
- An emergency medical team type 2 will be included as an emergency response capacity in the European Union’s civil protection pool and form part of the Emergency Medical Team (EMT) initiative, a network of medical teams qualified, trained and prepared to provide immediate assistance in the event of an emergency.
- A rapid response team for major burns and a specialist mother and baby unit will also be set up within the framework of the “rescEU EMT” consortium.
- The FPS Public Health will also provide medical support to all team members during B-FAST missions.
B-Fast in action
B-FAST’s most recent major medical operation was the post-earthquake operation in Turkey in 2023. Our country responded alongside France, Spain and Italy, sending a team of 207 volunteers, medical equipment to set up a EMT-2 type field hospital and a water treatment unit.
Due to the work of these volunteers, the field hospital was able to stay open 24 hours a day, 7 days a week from 16 February to 6 March 2023. The hospital, which included an emergency ward, a general consultation ward, a radiology service, a pharmacy and an operating room was able to help no fewer than 2,389 adults and 1,114 children, 400 of whom were aged under 5.

Despite B-FAST’s assistance, living conditions were particularly difficult for the affected population. In total, 491 of the 3,503 patients stayed in shelters, 2,295 patients lived in tents and 63 were sleeping in the street. Many of these patients did not have access to drinking water, food or toilets.
B-FAST recorded the most common complaints and shared them with the international community to improve its preparedness for future operations. In Turkey, the most common symptoms were, in decreasing order, respiratory problems and flu symptoms, localised cuts and fractures, gastro-intestinal disorders, skin problems and pain. This breakdown is observed after nearly all types of disaster.
These actions would not be possible without our pool of volunteers. This currently stands at 670 professionals, including medical and logistics profiles, but also experts in water purification and technicians.
Want to learn more?
https://www.health.belgium.be/en/b-fast
RescEU: million euros of medical assistance for Ukraine.
|
In March 2022, the European Commission and the FPS Public Health set up a platform in Belgium to transport privately-donated medication and medical equipment to Ukraine. This partnership, launched under the European Commission’s RescEU programme, was initially planned for a period of six months. However, as the need for medical provisions in Ukraine has persisted and the platform has continued to receive donations, the project has been extended. The project was first extended for six months, then a year. This partnership with the European Commission came at a crucial moment when the emergency situation in Ukraine required a united and coordinated response. This critical phase of the operation was concluded in February 2024, bringing to an end the project financed by the EU which facilitated the delivery of medical aid to Ukraine. This partnership set up with the EU will continue and the FPS Public Health will be ready to intensify its operations at any time, if the situation demands. Belgium will continue to support Ukraine with its own assistance and donations from third parties will be evaluated on a case-by-case basis. The European Commission will continue to transport private donations to Ukraine via its platform in Poland. |
“ Over the last two years, these donations worth over 5 million euros have been transported on more than 600 pallets. “ |
Want to know more?
https://civil-protection-humanitarian-aid.ec.europa.eu/what/civil-protection/resceu_en
[1]Source: National Crisis Centre (s.d.) Organisation in an emergency. https://crisiscenter.be/en/what-do-authorities-do/crisis-management/organisation-emergency
[2]The structure of the MIP is defined in a ministerial circular.
[3]Within the MIP, this is a temporary function held by a doctor who is in operational charge of all medical, sanitary and psychosocial support services at the site. This doctor works under the administrative authority of the Federal Health Inspector.
